What is Toenail Fungus?
Toenail fungus is one of the most common nail conditions worldwide. And it is important to find the best Toenail fungus treatment. Yet it is so often misunderstood. While many people first notice toenail fungus as a cosmetic issue, it is actually a medical condition that can worsen over time when left untreated. Due to the fact that toenail fungus infections develop slowly and are usually painless, it often goes unnoticed until the nails become really thick, discolored, and difficult to maintain.
Here we’ll discuss toenail fungus in its entirety. We’ll explain what toenail fungus is, how common it is, how people get it, available treatment options, preventative strategies, and geographic trends. Our goal is to help readers like you understand the condition clearly so you can make the most informed decision about your nail health.
Toenail fungus, medically known as onychomycosis, is a fungal infection that affects the nails. The fungi responsible for these infections feed on keratin, the protein that makes up the nail structure. Most cases are caused by dermatophytes, although yeast and mold can also be responsible.
The infection typically begins when fungal spores enter the nail through small cracks that are usually caused by trauma. Once inside, the fungus grows slowly under the infected nails, where it is protected from the outside environment. Because nails grow slowly, the infection can persist for months or even years without obvious symptoms.
At first, toenail fungus may appear as a small white or yellow spot. Over time, however, the nail may thicken, discolor, crumble, or lift from the nail bed. In advanced cases, the nail can become painful and permanently damaged. Toenail fungus differs from fingernail fungus in that toenails grow more slowly and are more often confined inside shoes, which creates an ideal environment for fungal growth. Therefore, toenail fungus is much more common than fingernail fungus.
Signs and Symptoms of Toenail Fungus
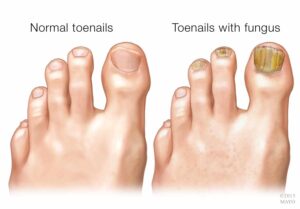
Toenail fungus symptoms can vary depending on how advanced the infection has become. In the early stages, the signs are often subtle and easy to overlook. Many people first notice small changes rather than discomfort. These early indicators may include faint white or yellow streaks on the surface of the infected nails, mild discoloration, or slight changes in nail texture. Because these symptoms develop gradually and are usually painless, they are frequently dismissed as minor nail damage or aging.
As the infection progresses, however, the symptoms typically become more noticeable and harder to ignore. The infected nails may begin to thicken and lose their smooth appearance. Over time, the structure of the nails weakens, making them brittle and more prone to cracking or crumbling at the edges. In addition, debris can accumulate beneath the nail plate, creating pressure and sometimes producing an unpleasant odor.
Common symptoms of toenail fungus include:
- White, yellow, or brown discoloration
- Thickened or hardened nails
- Brittle, cracked, or crumbly edges
- Distorted or misshapen nail appearance
- Debris buildup under the nails
- Nail lifting from the nail bed
- Foul odor in more advanced cases
In severe cases, the nail may turn dark brown or black and begin separating from the nail bed. At this point, the infection can cause discomfort, especially when wearing closed-toe shoes. Thickened nails may also make trimming difficult or painful. If left untreated, the nails can become permanently damaged or eventually fall off altogether.
How Common Is Toenail Fungus?
Toenail fungus is extremely common and affects people of all ages and walks of life. Studies estimate that approximately 10% of the general population has toenail fungus. However, prevalence increases significantly with age. Among adults over 60, rates rise to 20–32%, and among those over 70, the condition may affect more than half of the people. Men are more likely than women to develop toenail fungus, possibly due to footwear habits and occupational preferences. While toenail fungus is less common in children, it can still occur, especially in adolescents who participate in sports or swim frequently.
Toenail fungus accounts for nearly half of all nail disorders, making it one of the most frequently diagnosed nail conditions worldwide. Despite its prevalence, many people delay seeking treatment because early symptoms are subtle and painless.
Because toenail fungus develops slowly and often does not cause immediate discomfort, it is commonly not reported or treated. Several factors explain why toenail fungus affects so many people. Fungus thrives in warm, dark, and moist environments, conditions that shoes naturally create. When feet sweat inside shoes, moisture gets trapped, allowing fungi to grow and multiply. Additionally, fungal spores are widespread in public spaces such as locker rooms, gyms, pools, and communal showers. Walking barefoot in these environments increases exposure, especially if the skin or nails have small cracks. Another reason toenail fungus is so common is that nails grow slowly. Even when fungal growth is stopped, visible improvement depends on healthy nail growth, which takes months. This allows infections to persist unnoticed and untreated. Finally, many people mistake toenail fungus for nail trauma, aging, or cosmetic damage. As a result, treatment is often delayed until the infection becomes very severe.
How to Prevent Toenail Fungus
Preventing toenail fungus starts with understanding that fungal organisms thrive in warm, moist environments. Because your feet spend much of the day inside shoes, they are naturally more vulnerable to fungal infections. Fortunately, simple daily habits can significantly reduce your risk.
To protect your feet, follow these key prevention steps:
1. Keep Feet Clean and Completely Dry
Wash your feet daily with soap and water. Just as importantly, dry them thoroughly, especially between the toes. Even small amounts of trapped moisture can encourage fungal growth. If you sweat heavily, consider moisture-wicking socks and change them when necessary.
2. Choose Breathable Footwear
Shoes play a major role in prevention. Select footwear made from breathable materials that allow airflow. In addition, avoid wearing the same pair daily. Rotating shoes gives them time to dry completely between wears. You may also use antifungal powders or sprays inside shoes to further reduce moisture, bacteria, and fungus.
3. Protect Your Feet in Public Areas
Locker rooms, swimming pools, gyms, and communal showers are common sources of fungal exposure. Therefore, always wear sandals or shower shoes in shared spaces. This simple barrier significantly reduces your risk of contact with fungal spores.
4. Practice Proper Nail Care
Trim toenails straight across and avoid cutting them too short, as this can create tiny openings for fungus to enter. Always use clean, disinfected nail tools, and never share clippers, files, or footwear, even with family members.
5. Treat Athlete’s Foot Promptly
Because the same fungi can infect both the skin and nails, untreated athlete’s foot can easily spread to the toenails. Address skin infections early to prevent nail involvement.
By combining good hygiene, smart footwear choices, and consistent nail care, you can dramatically lower your chances of developing toenail fungus.
How People Get Toenail Fungus
Toenail fungus is not random. It happens to appear when fungus comes into contact with the skin or nails. Then it penetrates the surface into the nail structure itself.
Common ways people contract toenail fungus include walking barefoot in public places, wearing shoes that are too tight and don’t let feet breathe, and having sweaty feet. Small nail injuries or cracks also make it easier for fungus to enter and start multiplying.
Athlete’s foot is another major contributor. When fungal skin infections are left untreated, the fungus can spread from the skin to the nails. Sharing personal items such as socks, shoes, towels, or nail tools increases the risk of contracting a fungal infection.
Poor foot hygiene, including infrequent washing or improper drying, is also a factor. This may allow moisture to remain on the skin and nails, creating favorable conditions for fungal growth.
Risk Factors That Increase Susceptibility
While anyone can develop toenail fungus, certain factors certainly increase susceptibility. Age is one of the strongest risk factors, as nail growth slows down and circulation decreases over time, people get more susceptible to getting a toenail fungus infection and therefore need to find a treatment that works.
Also, medical conditions such as diabetes, poor circulation, immune suppression, and peripheral vascular disease increase risk as well. These conditions reduce the body’s ability to fight infection and heal damaged tissue.
Lifestyle is also a big factor. Athletes, people in the military, healthcare workers, and any other individuals who spend long hours in closed-toe shoes have higher exposure risks to a toenail fungus infection. Smoking, obesity, and repeated nail trauma further increase risk.
Having one or more risk factors does not guarantee infection, but it does make prevention and early detection especially important.
Diagnosis of Toenail Fungus
Although toenail fungus is common, it is not always easy to diagnose based on appearance alone. Many nail conditions can look similar, including psoriasis, nail trauma, bacterial infections, and age-related nail thickening. For this reason, proper diagnosis is important before beginning treatment.
Diagnosis usually begins with a clinical evaluation performed. Typically, a Podiatrist will examine the affected nails, looking for common signs such as discoloration, thickening, debris buildup, nail lifting, or distortion. The pattern of involvement can also provide clues. For example, fungal infections often begin at the tip or side of the nail and gradually spread inward. Additionally, fungus tends to spread from one nail to another, gradually over time.
In some cases, a visual exam may not be enough to confirm the diagnosis. To ensure accuracy, a small nail clipping or scraping from beneath the nail may be collected. This sample can then be examined under a microscope or sent to a laboratory for fungal culture or molecular testing. Laboratory confirmation helps determine whether fungus is present and can also identify the specific type of organism responsible. This method might seem the most accurate, but it is very difficult to take a sample in a sterile environment. So a lot of the times the test can come back with a false positive or negative result.
Accurate diagnosis matters because treating a non-fungal condition with antifungal medication will not improve symptoms. In addition, unnecessary treatment may expose individuals to avoidable costs or side effects. By confirming the presence of fungal infection before beginning therapy, patients can choose the most appropriate and effective course of action.
Treatment Options for Toeanail Fungus
The effectiveness of toenail fungus treatment depends on several factors, including the severity of the infection, nail thickness, and overall health. Because no single treatment works best for everyone, understanding the advantages and limitations of each option is essential.
1. Home Remedies
Some people begin with home remedies such as tea tree oil, vinegar soaks, baking soda, hydrogen peroxide, or menthol-based ointments. These options are inexpensive and easy to apply. In very mild cases, they may improve nail appearance or slow fungal growth. However, most home remedies cannot penetrate deeply enough to reach the fungus living under the nails. As a result, they rarely eliminate established infections and may only provide temporary cosmetic improvement.
2. Over-the-Counter (OTC) Topical Treatments
OTC antifungal creams, sprays, and medicated nail lacquers are widely available and simple to use. While they are generally safe, their cure rates are often low. This is because thickened nails act as a barrier, preventing the medication from reaching the infection at its source.
3. Prescription Topical Medications
Prescription-strength topical treatments offer stronger formulations than OTC products. Although they may improve effectiveness, they still require daily application for many months, often up to a year. Consistency is critical, and results depend on new nail growth.
4. Oral Antifungal Medications
Oral medications work systemically by traveling through the bloodstream to attack the fungus from within. They can be effective for moderate to severe infections. However, they may cause side effects and typically require medical monitoring during treatment.
5. Laser Treatment
Laser therapy uses focused light to target and kill fungus under the infected nails. When nails are significantly thickened, debridement (thinning of the nails) may be performed to improve penetration. This allows the laser to reach the infected nail bed more effectively.
Regardless of the method chosen, no treatment provides instant results. Successful therapy requires stopping fungal growth and allowing a healthy nail to grow out over time. Toenails grow slowly and typically take 6-9 months to fully replace themselves. Visible improvement appears gradually from the base of the nail. Even after the infection is eliminated, damaged portions must grow out completely.
For this reason, patience and consistent preventive care are essential to minimize the risk of recurrence.
Everything You Need to Know about Topical Medication for Toenail Fungus

Topical medications are often the first treatment people try for toenail fungus, especially in mild cases. These treatments include over-the-counter antifungal creams, sprays, solutions, and medicated nail lacquers, as well as prescription-strength topicals. The primary benefit of topical treatments is safety. Because these medications are applied directly to the nail and surrounding skin, they do not circulate through the bloodstream, which means they don’t have any systemic side effects. For individuals who cannot take oral antifungal medications due to liver concerns, medication interactions, or underlying health conditions, topical treatments may be a safer alternative. In addition, topical medications are non-invasive, easy to access, and generally well tolerated. They may also help prevent the spread of fungus in early infections or be used alongside other treatments as part of a combined approach.
However, topical treatments also have important limitations. The biggest challenge is penetration through the nail to the source of the infection. Toenail fungus lives under the nails, often deep in the nail bed, and thickened or damaged nails can act as a barrier that prevents any medication from reaching the root of the infection. As a result, cure rates for topical treatments alone are typically lower than those for oral medications. Consistency is another issue. Many topical treatments must be applied daily for several months, sometimes up to a year, and missing applications can reduce effectiveness. Additionally, visible improvement depends on new nail growth, which is slow, so results may take many months to appear even if the fungus has stopped growing. In moderate to severe cases, topical solutions alone may not clear the infection. Therefore, while topical medications can be beneficial for mild infections or for patients seeking a low-risk option, they may not always provide complete or lasting results when used alone.
Home Remedies for Toenail Fungus

Home remedies are a popular option for people who want to treat toenail fungus without prescription medications or medical procedures. Common home treatments include tea tree oil, vinegar soaks, baking soda, hydrogen peroxide, Vicks VapoRub, essential oils, and various natural antifungal solutions. The primary benefit of home remedies is accessibility. Most of these products are inexpensive, widely available, and easy to apply at home. In addition, some people prefer “natural” approaches because they avoid potential systemic side effects associated with oral medications. Some remedies may help reduce surface fungus, soften thickened nails, improve nail appearance slightly, or decrease odor. For very mild or early-stage infections, home care may slow progression or provide cosmetic improvement. Furthermore, certain practices such as soaking and trimming can make nails easier to manage and improve overall foot hygiene.
However, the limitations of home remedies are significant. The most important drawback is that most natural or DIY treatments cannot penetrate deeply enough to reach the fungus living under the nails in the nail bed. Toenail fungus is not just a surface issue. It often embeds itself in protected areas where topical household substances cannot effectively reach. As a result, home remedies rarely eliminate established infections and may only provide temporary improvement. Another concern is delayed treatment. Relying solely on home remedies for months can allow the infection to worsen, spread to other nails, or become more difficult to treat later. In some cases, improper use of substances such as undiluted essential oils, concentrated vinegar, or bleach can cause skin irritation, chemical burns, or permanent nail damage. For these reasons, while home remedies may play a supportive role in foot hygiene or very mild cases, they are generally not considered a reliable cure for moderate to severe toenail fungus.
Is Oral Medication a good option for you?
Oral antifungal medication is one of the most commonly prescribed treatment options for toenail fungus, particularly for moderate to severe infections. These medications work systemically, meaning they travel through the bloodstream to reach the infected nails from within your body. Because the medicine is taken internally, it can penetrate the nail bed more effectively than topical treatment options, which often struggle to pass through thick infected toenails. As a result, oral medications generally offer higher cure rates than over-the-counter creams, solutions, or lacquers. They can be especially helpful when multiple nails are affected, when the infection has spread significantly, or when the root of the nail is involved. Additionally, oral therapy does not require daily application to the nail surface, which some patients find more convenient compared to long-term topical regimens.
However, despite their effectiveness, oral antifungal medications also carry potential risks and limitations. These medications can affect liver function negatively, so healthcare providers often recommend multiple follow-up blood tests during the course of the treatment to monitor for liver enzyme changes. While serious complications are uncommon, possible side effects may include nausea, upset stomach, headaches, skin rashes, and, in rare cases, more severe reactions. Oral antifungals can also interact with other medications, making them unsuitable for some individuals, particularly those with liver disease, heart conditions, or certain chronic health issues. Treatment duration typically lasts a few months, and although the medication may stop fungal growth, visible improvement still depends on slow nail regrowth, which can take 6-9 months. For these reasons, while oral antifungal therapy can be an effective option, the decision to use it should be based on a careful evaluation of potential benefits and risks.
Laser Treatment for Toenail Fungus
Laser treatment is the newest treatment option. This technology-based treatment for toenail fungus has gained attention as an alternative to oral and topical medications. This approach uses focused light energy that passes through the nails and uses heat to kill the fungus. The primary benefit of laser treatment is that it targets the infection directly without requiring systemic medication. Because it does not circulate through the bloodstream, it avoids the liver-related risks and drug interactions associated with oral antifungal medications. This treatment is the safest option for almost all patients. In addition, laser therapy is non-invasive, does not require anesthesia, and has no downtime. During the treatment, patients describe the sensation as warmth or mild tingling rather than pain. Another advantage is convenience: treatments are performed in-office and do not rely on daily at-home application. Laser treatment for toenail fungus may be particularly appealing to people who are not able to take oral medications or who have not responded to topical treatments.
However, laser treatment also has limitations that should be considered. While many patients experience improvement, outcomes can vary depending on the severity of the infection, nail thickness, and overall health. In some cases, multiple sessions may be required, and visible results still depend on slow nail regrowth, which can take 6-9 months. Additionally, laser treatment is not covered by insurance. This makes cost a factor for some individuals. Although side effects are generally minimal, temporary warmth, mild redness, or slight discomfort can occur. As with any treatment option, success also depends on proper foot hygiene and prevention of reinfection. Therefore, while laser therapy offers a medication-free and non-invasive approach to treating toenail fungus, it is most effective when chosen thoughtfully and combined with good post-treatment care.
Preventing Recurrence of Toenail Fungus
Even after toenail fungus has been successfully treated, preventing recurrence is essential. Reinfection is common because fungal spores are widespread in the environment and can remain in shoes, socks, and shared spaces. Without consistent preventive measures, the same conditions that allowed the infection to develop initially can quickly lead to another outbreak.
To reduce the risk of recurrence, follow these key strategies:
1. Maintain Strict Foot Hygiene
Wash your feet daily with soap and water. Just as importantly, dry them thoroughly, especially between the toes. Moisture control remains critical even after the infection clears. Wearing moisture-wicking socks and changing them promptly if they become damp can significantly reduce fungal growth.
2. Manage Your Footwear Carefully
Rotate your shoes daily to allow them to dry completely between uses. Disinfect footwear regularly using antifungal sprays or ultraviolet shoe sanitizers to eliminate lingering spores. If certain shoes were heavily worn during the infection and retain odor or moisture, consider replacing them.
3. Sanitize Personal Items
Socks worn during active infection should be washed in hot water to help kill residual fungi. Nail tools used during the infection should be disinfected thoroughly or replaced altogether. Avoid sharing nail clippers, files, or footwear with others.
4. Protect Your Feet in Public Spaces
Continue wearing sandals or shower shoes in locker rooms, swimming pools, gyms, and communal showers. Even after treatment, exposure to contaminated surfaces can reintroduce fungus to your nails.
5. Monitor Nail Health Closely
Pay attention to early signs such as discoloration, thickening, or texture changes. Acting quickly at the first sign of recurrence can prevent the infection from becoming established again.
By combining diligent hygiene, smart footwear practices, environmental cleaning, and early vigilance, you can greatly reduce the likelihood of toenail fungus returning after treatment.
Complications of Untreated Toenail Fungus
While toenail fungus may begin as a cosmetic concern, it can lead to complications if left untreated. Because fungal infections tend to persist and gradually worsen, early management is often easier than addressing advanced disease.
One of the most common complications is spread. The infection can move to additional toenails or even to the surrounding skin, leading to athlete’s foot. In some cases, fungus may also spread to fingernails, particularly if hygiene practices are inconsistent.
As the infection progresses, nails may become significantly thickened and deformed. This thickening can create pressure inside shoes, leading to discomfort or pain during walking. Over time, difficulty trimming the nail may increase the risk of ingrown nails or secondary bacterial infections.
For individuals with underlying health conditions such as diabetes or circulatory disorders, untreated toenail fungus can pose additional risks. Cracked skin and thickened nails may create entry points for bacteria, increasing the likelihood of cellulitis or more serious soft tissue infections.
Advanced infections can also result in permanent nail damage. The infected nails may become distorted beyond repair or detach entirely from the nail bed. Because toenails grow slowly, recovery from severe damage can take many months.
Although toenail fungus is rarely life-threatening, allowing it to progress unchecked can lead to discomfort, complications, and more complex treatments later.
Lifestyle Impact of Toenail Fungus
Toenail fungus affects more than just your nails — it can disrupt your emotional well-being and daily life. Because nails are visible, even mild discoloration or thickening often creates embarrassment. Many people avoid open-toed shoes, sandals, swimming pools, and social situations where others might see their feet.
Athletes and active individuals often struggle with performance issues caused by nail fungus. Thickened nails create discomfort inside tight athletic shoes, and distorted nails make long periods of activity painful. Over time, that discomfort limits workouts and reduces participation in sports.
In professional environments, visible nail changes can undermine confidence. People who work in settings that emphasize grooming and presentation often feel self-conscious about their appearance.
The chronic nature of toenail fungus also creates frustration. Treatment requires patience, and visible improvement takes time. When recurrence happens, it can intensify disappointment and discouragement.
Toenail fungus remains medically manageable, but its effects reach beyond physical symptoms. Treating both the infection and the emotional impact improves overall quality of life. Open conversations and clear expectations about treatment timelines help reduce anxiety and frustration throughout the process.
This article was written by Dr. Jay Seidel, DPM, a board-certified podiatrist practicing in Baltimore, MD, and Southern Florida. Dr. Seidel has extensive experience diagnosing and treating foot and nail conditions, including laser treatment for toenail fungus.





